Scoliosis
the complete guide
- Published on
- By New Equilibre
When you or a loved one is faced with scoliosis, it's natural to want to understand the condition and explore the best treatment options.
In this comprehensive guide, we'll look in detail at what scoliosis is, its symptoms, causes, available treatments, the use of orthopedic inserts, as well as answer frequently asked questions to help you better manage this condition.
What is scoliosis?
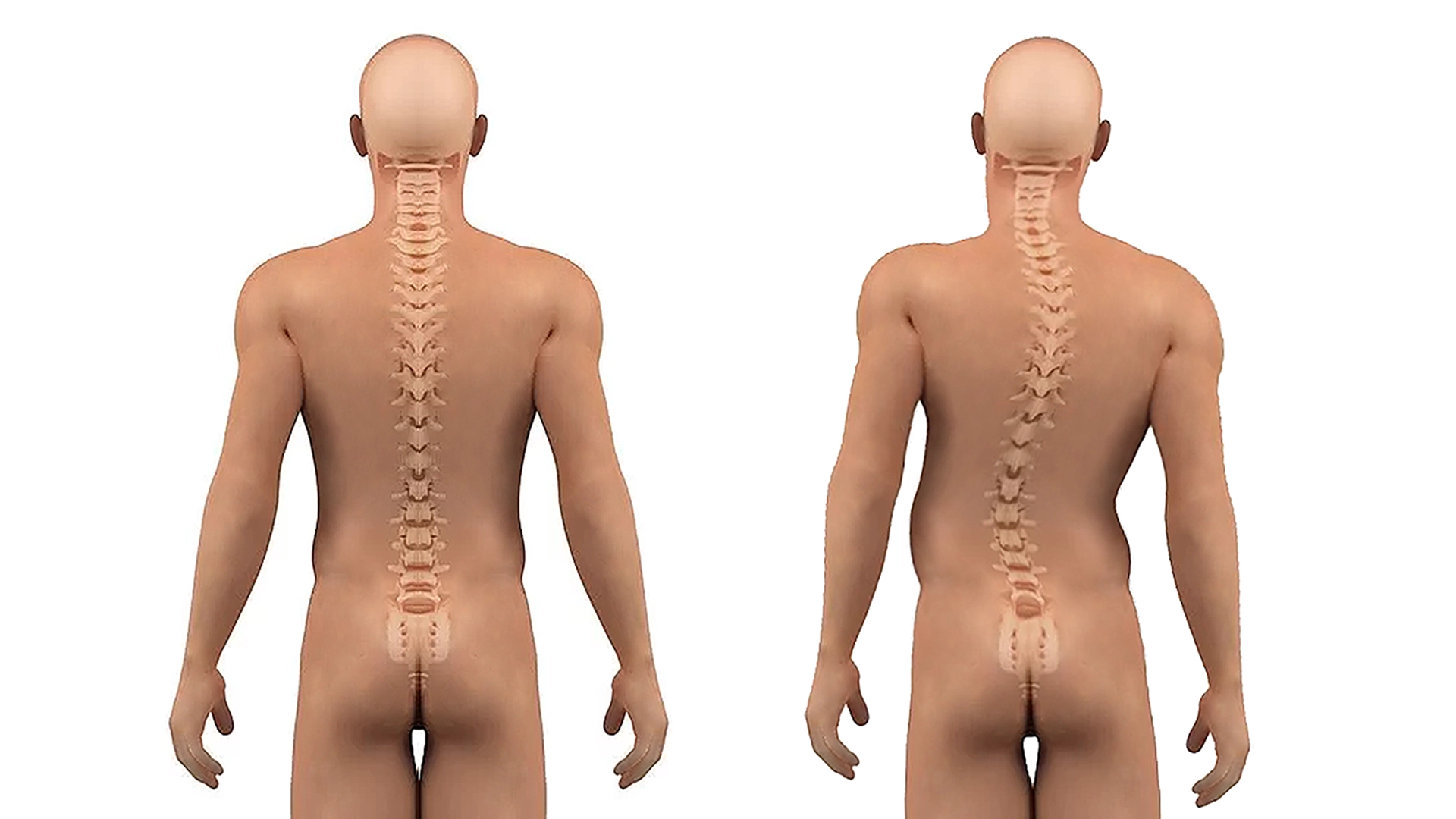
Scoliosis is a spinal deformity characterized by abnormal lateral curvature. Normally, the spine has natural curves that allow it to support the body and distribute weight evenly. However, in scoliosis, the spine presents an excessive lateral curvature, forming an "S" or "C" rather than a straight line.
This pathology can develop at different stages of life, but is often diagnosed during childhood or adolescence, when growth is rapid. Scoliosis can be mild, moderate or severe, and its severity depends on factors such as the patient's age, the location and degree of curvature, and the presence of associated symptoms.
It can lead to complications if left untreated, including back pain, body asymmetry, respiratory problems, heart problems and impaired lung function. It is therefore essential to consult a healthcare professional as soon as signs of scoliosis are detected for an accurate diagnosis and appropriate treatment plan.
What are the symptoms of scoliosis?
The symptoms of scoliosis can vary depending on the severity of the spinal curvature and the presence of other associated complications. However, here are some common symptoms that may indicate the presence of scoliosis:
Body asymmetry: Scoliosis can cause visible asymmetry, such as shoulders or hips that appear to be misaligned or higher on one side than the other.
Scapula asymmetry: The shoulder blades can appear to be at different heights when you look at them from behind.
Asymmetrical waist: One leg may appear longer than the other, or the pant size may appear uneven.
Back pain: People with scoliosis may experience back pain, particularly in the area where the spine is curved.
Muscle fatigue: The muscles of the spine can tire more quickly in people with scoliosis due to the strain placed on them to compensate for the curvature.
Difficulty breathing: In severe cases of scoliosis, the curvature of the spine can cause compression of the lungs, which can make breathing difficult.
It's important to note that some cases may be asymptomatic, especially if they're mild.
What causes scoliosis?
The exact cause of scoliosis is not always clear-cut, but it can result from a variety of factors, including:
Genetic factors: It can sometimes be hereditary, meaning it can be passed from parent to child. Research suggests that there are genes that can predispose a person to developing scoliosis.
Congenital anomalies: Some people may be born with scoliosis due to congenital spinal abnormalities, such as irregular vertebrae or defects in formation.
Rapid growth: Scoliosis can develop during periods of rapid growth, such as childhood and adolescence. During these periods, the spine may be more prone to deformity.
Muscle imbalances: Muscle imbalances or abnormalities in the back muscles can also contribute to the development of scoliosis by exerting uneven traction on the spine.
Environmental factors: Certain environmental factors can also play a role in the development of scoliosis, such as carrying heavy backpacks on one shoulder, poor posture, or excessive use of electronic devices.
It's important to note that in many cases, the specific cause of scoliosis may be unknown, and can vary from person to person. The management of scoliosis will depend on a number of factors, including the severity of the curvature, the patient's age and the presence of associated symptoms.
How can I stop scoliosis from progressing?
Stopping the progression of scoliosis isn't easy, but several approaches can slow or stabilize the progression of spinal curvature. Here are just a few of the strategies that can help stop or slow its progression:
Regular medical follow-up: Regular visits to a doctor or spine specialist are essential to monitor the progression of scoliosis. Regular examinations will detect any changes in the curvature of the spine and adjust the treatment plan if necessary.
Physiotherapy and specific exercises: Targeted muscle-strengthening and flexibility exercises can help stabilize the spine and strengthen the muscles that support posture. A physiotherapist can recommend specific exercises tailored to each patient's situation.
Wearing an orthopedic corset: In cases of moderate to severe scoliosis, wearing an orthopedic corset may be recommended to help maintain the curvature of the spine and prevent it from worsening. The corset is usually worn for several hours a day, particularly during rapid growth in childhood and adolescence.
Spinal fusion surgery: In severe cases of scoliosis, when the curvature of the spine is severe and other treatments have failed to control the progression of the curvature, spinal fusion surgery may be recommended. This procedure involves fixing the vertebrae together using materials such as rods, screws and bone grafts to stabilize the spine and correct the curvature.
Maintaining good posture and healthy lifestyle habits: Adopting good posture and avoiding activities that can aggravate scoliosis, such as carrying heavy backpacks over one shoulder, can help slow the progression of spinal curvature.
It's important to note that the effectiveness of different treatments can vary according to the severity of the scoliosis and the individual needs of each patient. It is therefore advisable to consult a doctor or spine specialist for personalized advice on the best treatment approach for each specific case of this pathology.
Orthopedic insoles to relieve scoliosis
Orthopedic insoles, also known as foot orthotics, can be an important part of scoliosis treatment. They are used to help correct postural imbalances and relieve pain associated with scoliosis by supporting the feet and reducing muscular and tendon tension.
Postural correction: Orthopedic insoles are designed to correct biomechanical imbalances that can slow and relieve scoliosis. They can help stabilize the feet, correct defects in pronation or supination, and realign the lower limbs, which can contribute to better overall posture and reduced strain on the spine.
Pain reduction: Orthotics can help reduce the pain associated with this condition by evenly distributing pressure on the feet and supporting the plantar arches. They can also help reduce muscular tension in the back, hips and legs by improving body alignment.
Improved stability: By providing extra support to the feet, orthotics can help improve stability and balance, which can be beneficial for people with scoliosis who may have reduced mobility or impaired coordination.
Preventing complications: By maintaining better posture and reducing muscle tension, orthopedic inserts can help prevent long-term complications of scoliosis, such as premature osteoarthritis or degenerative spinal disorders.
Free delivery to Metropolitan France, within 2 working days.
Free returns within 14 days.
When does scoliosis stop?
Scoliosis can develop at different stages of life, but in general, growth of the spine stops at the end of adolescence, when the bones have matured and bone growth is complete. However, it is important to note that it can continue to progress in some individuals even after growth has ceased, particularly in cases where spinal curvature is severe.
For most people with idiopathic scoliosis, the most common form of scoliosis with no identifiable cause, the progression of spinal curvature tends to slow and stop once bone growth is complete. This usually occurs in late adolescence, around age 16 to 18 in girls and 18 to 20 in boys.
However, it's important to note that scoliosis can continue to progress in some individuals even after growth has ceased, particularly in cases where the curvature of the spine is severe or where there are risk factors such as muscle imbalances, poor posture or overuse of the spine. This is why regular medical follow-up is often recommended to monitor the progression of scoliosis and adjust the treatment plan if necessary.
What makes scoliosis worse?
Several factors can aggravate scoliosis or contribute to its progression. Here are some of the main factors:
Bad posture: Adopting poor posture can put additional pressure on the spine and aggravate existing curvature.
Overweight: Excess weight can lead to additional pressure on the spine, which can worsen the curvature of scoliosis.
Supporting heavy loads: Regularly carrying heavy backpacks on one shoulder or carrying unevenly distributed loads can put uneven pressure on the spine and aggravate scoliosis.
High-impact activities: Some high-impact physical activities, such as jumping, running or contact sports, can put extra pressure on the spine and increase the risk of scoliosis progression.
Genetic factors: Although scoliosis is not entirely genetic, there are genetic predispositions to developing this condition. A family history of scoliosis can increase the risk of developing the condition.
Misuse of the spine: Adopting poor postural habits in daily life, at work or at school can put additional pressure on the spine and aggravate pathology.
Advanced age: In some older people, scoliosis may progress due to degenerative changes in the spine associated with aging.
It's important to note that some of these factors can be controlled or modified to reduce the risk of scoliosis progression. For example, adopting good posture, maintaining a healthy body weight, avoiding asymmetrical heavy lifting and engaging in gentle physical activity can help manage scoliosis and prevent its progression.
Is scoliosis a long-term condition?
In France, scoliosis can be considered as an Affection de Longue Durée (ALD) in certain cases, notably when it leads to significant functional limitations requiring regular medical monitoring. ALD conditions require prolonged treatment and regular medical supervision. They are specifically covered by the Assurance Maladie, which may include the cost of medical care, examinations, treatments and medical devices required to manage the disease.
However, not all forms of scoliosis are automatically considered ALD. The decision to recognize scoliosis as an ALD will depend on the severity of the condition, its impact on the patient's daily life, and the need for regular medical follow-up. This decision is taken by the treating physician in collaboration with the Assurance Maladie, according to criteria defined by French legislation.
It is therefore advisable to consult a doctor to obtain a precise assessment of the pathology and to determine whether it can be considered an ALD. If this is the case, the patient can benefit from specific treatment and access to medical care adapted to the management of his or her condition.
What's the best sport for scoliosis?
Choosing the best sport for people with scoliosis will depend on a number of factors, including the type and severity of spinal curvature, associated symptoms, and the individual's personal preferences. However, certain sports and physical activities can be particularly beneficial for strengthening back muscles, improving posture and promoting overall spinal health. Here are just a few examples:
Swimming: Swimming is often recommended for people with scoliosis, as it strengthens back muscles and improves spinal flexibility without putting undue pressure on joints.
Yoga and Pilates: These disciplines focus on strengthening core muscles, flexibility and correcting posture, which can be beneficial for people with scoliosis.
Walking: Walking is a low-impact activity that can help strengthen back muscles and improve posture without undue stress on the spine.
Cycling: Cycling, especially on a stationary or upright bike, can be a good option for strengthening back muscles and improving cardiovascular health.
Gentle gymnastics: Some forms of gentle gymnastics, such as stretching or tai chi, can help improve flexibility, balance and coordination, which can be beneficial for people with scoliosis.
It's important to note that everyone reacts differently to physical activities, so it's advisable to consult a doctor or spine specialist before starting a new exercise program, especially in cases of scoliosis. A health professional will be able to recommend activities suited to each individual's specific situation, and provide advice on how best to perform them safely.

New Equilibre
Healthcare professionals specializing in the manufacture of orthopedic insoles for over 30 years. Clinically proven expertise with thousands of New Equilibre users and patients in orthopedic practices.

